Home
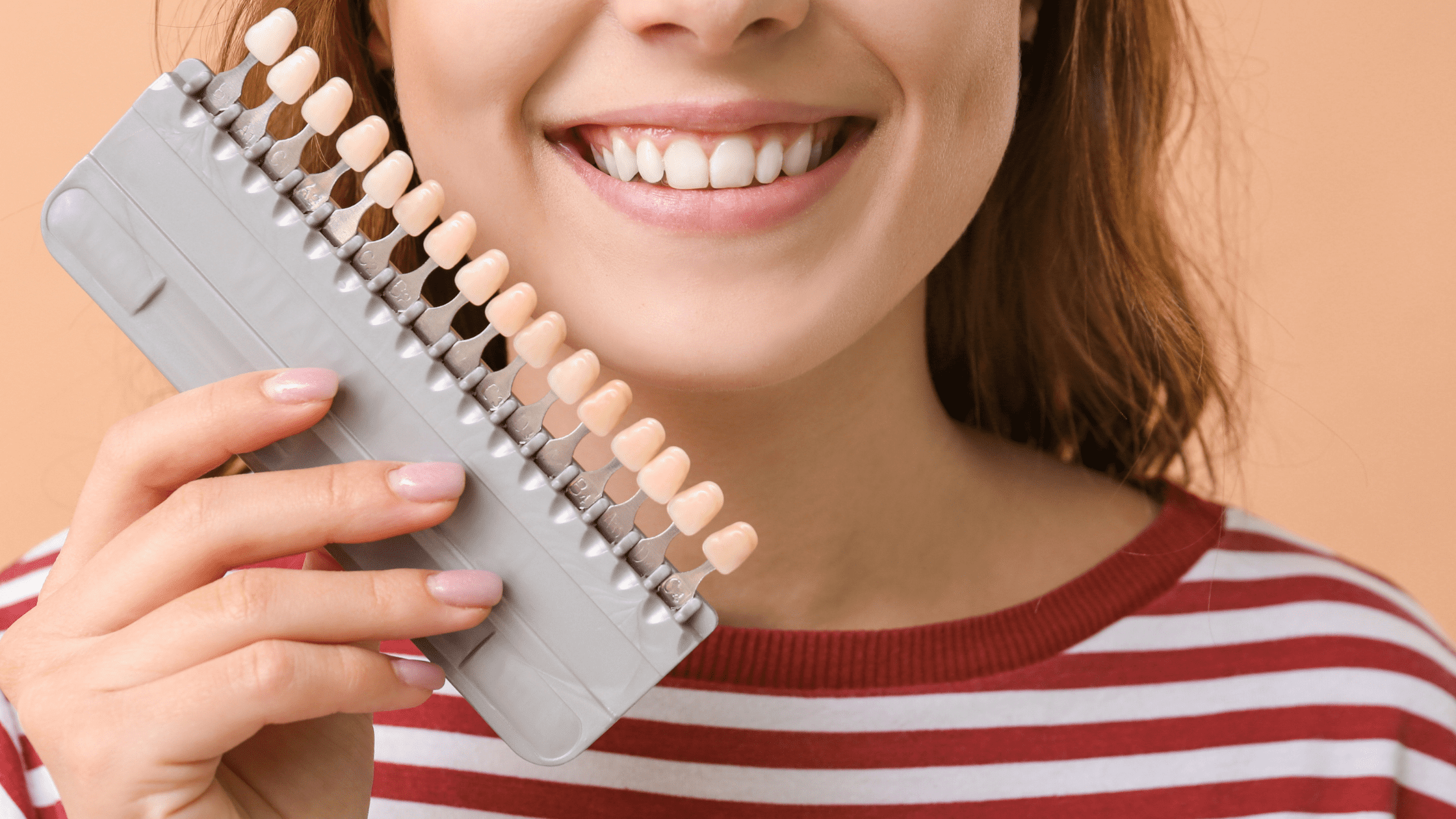
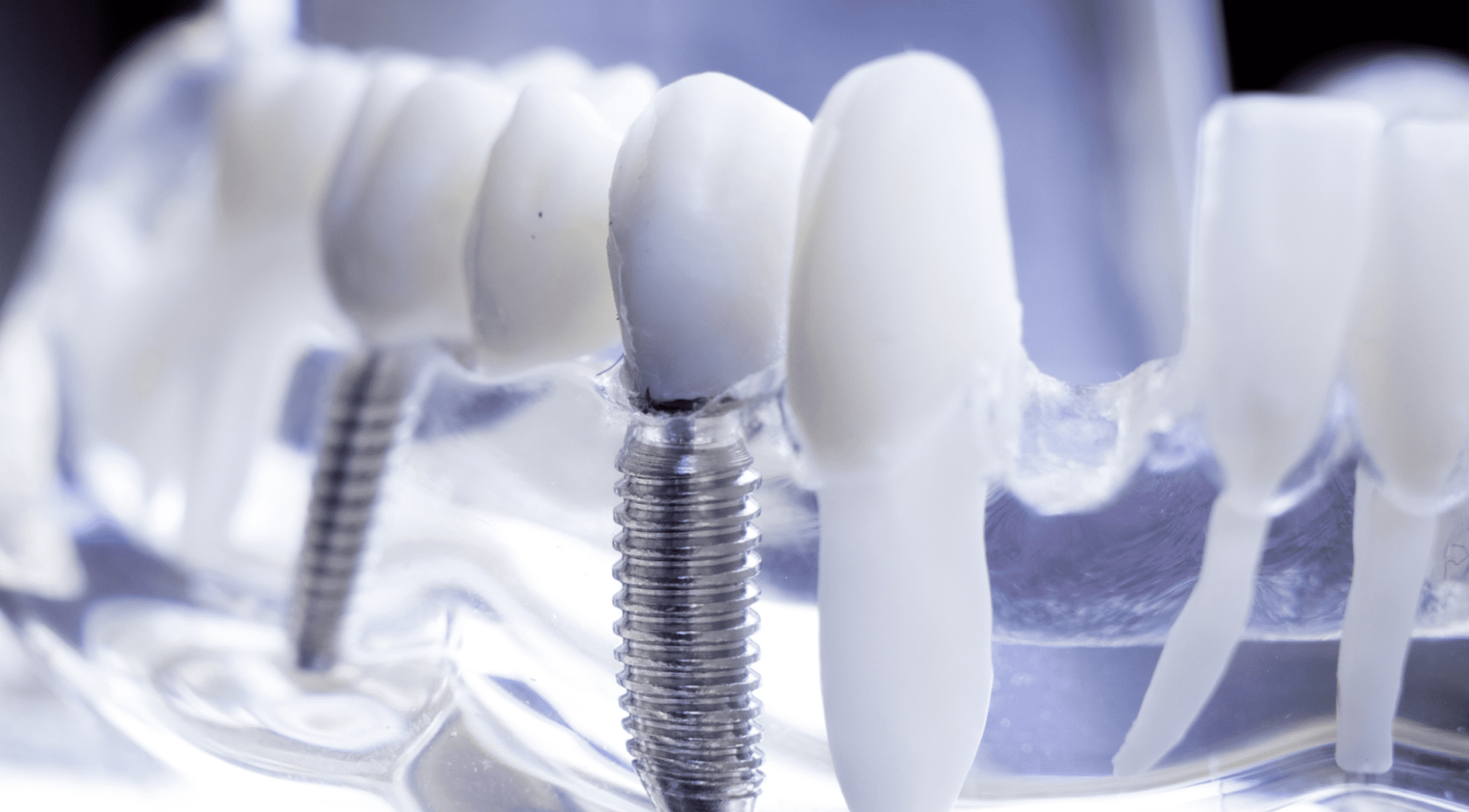
Dental ImplantsImplant Supported DenturesGeneral DentistryWisdom TeethOrthodonticsVeneersRoot CanalFillingsPediatric Dentistry
Dental ImplantsNew PatientOur TeamContact UsBook an Appointment
Mon & Fri:
9 AM - 5 PM
9 AM - 5 PM
Tue & Wed:
9:30 am - 7 pm
9:30 am - 7 pm
Thurs:
10 AM - 5 PM
10 AM - 5 PM
Sat:
10 am - 4 pm
10 am - 4 pm
Sun:
Closed
Closed
2975 Glen Dr, Coquitlam, BC V3B 2P7